High Arches Causing You Trouble?
A Real-Life Case Study on Cavus Foot Gait Dysfunction
From The Body Lab, Canberra
Foot pain. Calluses. Tight hips. Knees that complain every time you squat. If you’ve got high arches (aka pes cavus) and your body feels like it’s compensating with every step, you’re not alone—and you’re definitely not broken.
At The Body Lab in Canberra, we help people reclaim their mobility by improving the way they move—starting from the ground up. And no, orthotics aren’t the only answer.
This real-life case study dives into what happens when high arches go ignored, and how we helped one client move from pain to performance.
Meet Debbie
Debbie came to us with a history of:
Right foot surgery in 2020 (peroneal tendon repair + arch modification)
Chronic foot tension and callus formation under her big toe
Arthritis in both knees and her left hip
A walking pattern that left her feeling stiff, sore, and unsupported
Her goal? Walk pain-free and ditch the constant tension.
She had been using orthotics daily to “force her feet to pronate”—but they weren’t solving the problem. Just masking it.
Why Are High Arches a Problem?
A high arch means your foot doesn’t flatten much during walking. Sounds stable, right? But a rigid, supinated foot:
Doesn’t absorb shock properly
Loads pressure into the outer foot
Disrupts gait mechanics all the way up the chain
Over time, this leads to:
Lateral foot pain
Clawing toes
Bunions
Knee dysfunction
Hip and pelvic tension
And yes—chronic over-reliance on orthotics
Debbie’s Biomechanical Assessment
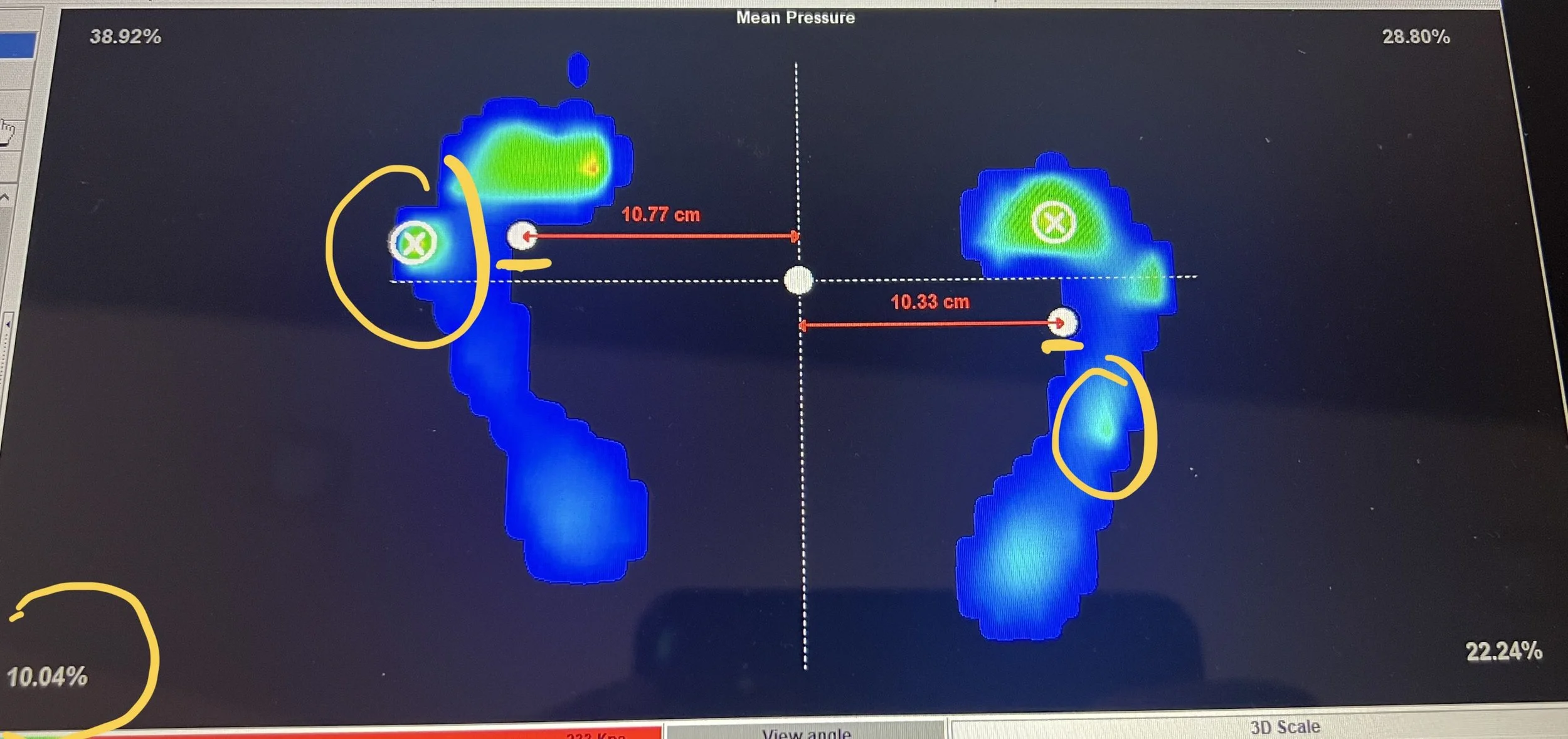
before treatment analysis
Here’s what we found during her full-body gait and posture analysis:
1. Postural Assessment
Feet: High arches, with heels turned out (everted) and forefoot twisted inward
Right foot more affected, with bunion signs and thick callus under the 1st toe and MTP joint
Right tibia rotated in, right knee bent and internally rotated
Left leg showed external knee rotation
Pelvis tilted left, elevated right, rotated left, and shifted forward—placing her centre of mass over her toes
Thoracic spine flattened; neck over-extends to compensate
2. Static Pressure Plate Findings
Just 10% of weight in left heel (ideal = 25%)
Excessive load in right forefoot, especially cuboid and 5th met head
Centre of mass biased forward and rotated left
Left foot shifted forward; right foot pulled back
3. Dynamic Pressure Plate Analysis
Initial Contact: Right foot lands on the inside of the heel (not ideal); left foot lands centrally
Loading Phase: Right loads from heel → cuboid → 5th toe (skipping the big toe entirely)
Midstance: Right foot stuck in mid-forefoot; left foot pressure sits laterally
Push-Off: No big toe pressure in either foot = lost propulsion
more about ‘Pressure Plate Gait Analysis Canberra”
4. Gait Video Analysis
Right arm swings outward, trunk leans forward—classic compensation
No hip extension or spinal side-bend during right leg loading
Knees and ankles lack fluid movement
Pelvis remains off-centre throughout gait cycle
5. Movement & Mobility Assessment
Pelvis: Limited tilt and rotation; right-sided drop
Spine: No thoracic flexion, extension, or left-side movement
Right ankle: Lacks internal rotation = poor limb loading
Head: Restricted in all planes of motion
What We Did (And Why It Worked)
1. Centre of Mass Reset (Spinal Mobility)
We used segmental spinal drills to bring movement back to her thoracic and lumbar spine—restoring flexion/extension and helping her shift her weight back into the heels where it belongs.
Goal: De-load the toes, re-centre her pelvis, and reconnect the spine to the feet.
2. Foot Pronation Drills (Arch Drop)
Debbie’s feet had forgotten how to share the load.
We introduced arch drop exercises to retrain the foot’s natural pronation response—without collapse.
Cue: Keep your heel grounded, allow the arch to soften, let the shin glide forward and inward.
This movement allowed her forefoot and midfoot to finally participate.
3. Ankle Rotation & Realignment
The right ankle had lost its ability to rotate inwards—so the knee and hip were compensating.
We used internal ankle rotation drills to:
Improve knee tracking
Restore pelvic balance
Set up more efficient propulsion during gait
Debbie’s Movement Plan
Daily Reps:
Feet: 2–5 reps, 5x per day
Spine: 5 reps, 5x per day
Reminder: These are awareness drills—not workouts. The goal is nervous system retraining, not exhaustion.
What Changed After One Session?
After Treatment analysis
Debbie felt more grounded, with weight spread across her full foot (not just the pinky toe)
She could finally feel big toe engagement during walking
Gait video showed reduced arm swing, better hip control, and less trunk sway
Most importantly?
She left the session feeling freer, lighter, and confident about taking her first steps toward pain-free movement.
Clinical Takeaway:
High arches aren’t just a foot issue. They affect:
Your posture
Your pelvic stability
Your ability to walk and run without strain
Orthotics can support the structure—but only movement retraining can restore function.
Ready to Fix Your High Arches?
If you’ve been walking on the outside of your feet, gripping the ground with your toes, or wondering why your hips always feel tight… it might be time for a proper foot and gait assessment.
👣 Book Your Assessment Now
📍 Canberra-based? Click below to book your session:
👉 Book your Advanced Biomechanical Assessment
Or contact me for a free 15-minute discovery call to chat about your goals.
Bonus: Support The Body Lab
Did this story resonate with you?
If you’ve worked with us, we’d love your feedback. Your reviews help others find foot-friendly, movement-first therapy that actually works.